Fungal infections happen when certain types of fungi grow too much on or inside the body. While many fungi naturally exist in harmless small amounts, problems arise when their numbers increase excessively or when new types of fungi are introduced.
One common cause of fungal infections is acrylic nails, those plastic nails stuck onto real ones with glue. Although usually not a big deal, acrylic nails can sometimes lead to fungal infections in the fingernails. Luckily, these infections usually clear up fine with home remedies or antifungal meds.
This article will discuss how acrylic nails can lead to fingernail fungal infections, how to treat these infections effectively, and what steps can be taken to prevent them from happening again.
What Is Green Fungus Under Acrylic Nails?
Green fungus under acrylic nails occurs when a certain type of bacteria called Pseudomonas aeruginosa builds up beneath the nail. This bacteria is responsible for the greenish discoloration often seen in such cases. Pseudomonas aeruginosa is commonly found in both fresh and saltwater environments, particularly in areas like swimming pools, hot tubs, bathtubs, and showers.
This bacteria thrives in damp, poorly ventilated environments, similar to how moss grows in an unclean fish tank. Consequently, it can flourish under artificial nails where moisture gets trapped, leading to the development of green fungus.

Notes: Remember to keep your nails clean and dry to lower the chance of fungal infections. Avoid keeping your nails wet for too long and don’t overdo it with acrylic nails. Also, make sure the nail salon you visit follows good hygiene practices and uses clean tools to reduce the risk of fungal contamination.
How Does Nail Fungus Form Under Acrylic Nails?
Nail fungal infections account for over half of all nail problems and are especially common among individuals who wear acrylic nails. In a study involving 68 women with nail issues following acrylic nail removal, a staggering 67 of them were diagnosed with fungal infections.
Acrylic nails are attached to natural nails with a special glue. If they loosen or aren’t applied correctly, moisture can get trapped between the artificial and the natural nails. This moisture creates an ideal environment for fungi to grow, which can result in a fungal infection of the nail.
Among the various types of fungi, dermatophytes are the primary culprits behind nail fungal infections, with the fungus Trichophyton rubrum being particularly prevalent.

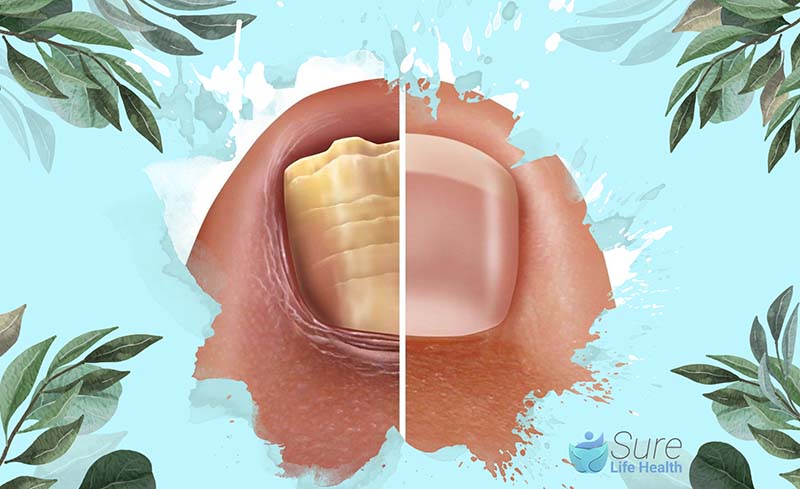
Typical Signs of Green Fungus Under Acrylic Nails
Initially, a fungal infection may not show any noticeable symptoms, but as it progresses, the following signs may become evident:
- Brittle or thickened nails
- Unpleasant odor emanating from the affected nail
- Pain and tenderness, particularly when applying pressure to the nail
- Discoloration of the nail, appearing yellow, green, black, or white
- Itchiness
- Redness
- Swelling
How to Get Rid of Nail Fungus From Fake Nails
If you develop green nails, it’s essential to first remove any remaining gel or acrylic to check if other nails are affected. The bacteria causing the green nail can be effectively eliminated with alcohol, making the treatment straightforward.
However, while the green stain may persist, it’s important to note that the bacteria is no longer contagious once eradicated.
In cases where green nails are accompanied by conditions like Onycholysis (separation of the nail from the nail bed) or ingrown nails, or if there are other concerns about nail health, it’s advisable to seek medical attention.
Individuals with weakened immune systems, underlying illnesses, or advanced age should especially consult a doctor if any abnormalities are noticed with their nails.
How to Prevent Nail Fungus Under Acrylic Nails
To minimize the risk of fungal infections when wearing acrylic nails, it’s important to prepare and care for your nails properly:
- Start with Clean, Dry Nails: Before applying acrylic nails, make sure your natural nails are thoroughly clean and completely dry. Check for any signs of infection or damage on your nails and treat any cuts to avoid bacteria entering through open wounds.
- Be Cautious with Water Exposure: Avoid soaking your nails in water for long periods during the application of acrylic nails, as excessive moisture can encourage fungal growth. If you plan to swim or participate in activities where your hands will be submerged, consider wearing waterproof gloves and always dry your hands thoroughly afterward.
- Maintain Nail Hygiene: Regularly trim your nails to prevent bacteria and fungi from finding places to thrive. After filing your nails, use an antifungal solution, such as tea tree oil, to disinfect the area. This step helps in further reducing the risk of developing a fungal infection.
By following these straightforward steps, you can enjoy your acrylic nails while keeping your natural nails healthy and free from infections.

Side Effects Caused by Acrylic Nails
While many individuals using acrylic nails won’t encounter serious issues, there are instances where they may cause allergic reactions or other adverse effects.
Allergic Reactions and Eczema: Some people acrylic nails may develop contact dermatitis, an allergic reaction akin to eczema. This reaction can stem from the artificial nails themselves or the adhesive used to attach them. Research from 2022 highlighted that exposure to acrylic nails could contribute to hand eczema, affecting both users and beauty professionals.
Symptoms of hand eczema may include redness, itching, peeling, cracked or scaly patches, and dryness. It’s crucial for those experiencing these symptoms after acrylic nail contact to consult a doctor. Healthcare professionals may prescribe medications or suggest over-the-counter remedies to manage eczema. They might also advise against further use of acrylic nails.
Nail Damage: Acrylic products can harm the nails, potentially leading to “worn-down nail syndrome,” characterized by nail thinning following exposure to acrylics and filing. A 2020 case study documented a woman exhibiting nail damage after acrylic use, manifesting symptoms like onycholysis (nail separation from the nail beds) and red, thickened skin around the nails.

Other Safety Concerns: Acrylic nails possess flammable properties, which require careful handling. Individuals wearing acrylic nails may have a tendency to pick at them, potentially leading to damage of the natural nail plate. Such actions can thin the nails and result in flaking or pitting on their surfaces. It is advisable to be aware of these risks and exercise caution when managing acrylic nails.
When to Go to the Hospital?
While most nail fungal infections resolve with home remedies, it’s wise to consult a doctor if these measures prove ineffective or if the infection causes significant discomfort.
Additionally, individuals who are immunosuppressed should consider seeking medical advice to prevent the development of more severe infections.
If you fall into this category or if your symptoms persist despite home treatment, it’s prudent to schedule an appointment with a healthcare professional for further evaluation and possible prescription of antifungal medications.

Conclusion
Fungal infections arising from acrylic nails are a prevalent issue, often triggered by trapped moisture beneath the nails, fostering excessive fungal growth.
Fortunately, most fungal infections associated with acrylic nails are not severe and can be effectively managed at home. In cases of more serious infections, prescription antifungal medications typically offer successful treatment outcomes.
Be sure to explore more insightful blogs from Sure Life Health, where we continue to shed light on the latest trends and breakthroughs in health and wellness.
Professor Gaye Cunnane, PhD, MB, FRCPI
As the Director of Health and Wellbeing at RCPI, Professor Gaye Cunnane is at the helm of initiatives aimed at enhancing the health and well-being of RCPI Trainers and Trainees. Her role extends beyond administration; she is also a respected clinical professor of rheumatology and a consultant rheumatologist at Trinity College Dublin (TCD) and St James’s Hospital. Prof. Cunnane’s medical journey began at TCD, where she graduated from medical school, and her path has been marked by both clinical and academic excellence.
After completing her basic clinical training in medicine, she embarked on PhD studies at University College Dublin and St Vincent’s University Hospital. Her research during this period was focused on prognostic markers in early inflammatory arthritis, a project that saw her collaborating with esteemed universities across Europe, including in Switzerland, The Netherlands, the UK, and Sweden.
Prof. Cunnane’s career took her to the University of California, San Francisco, where she spent three years delving into research on new treatments for lupus. Her academic prowess led her to the University of Leeds in 2001 as a senior lecturer, before returning to Ireland in 2003 to assume her current roles. She has also served as the National Specialty Director for Rheumatology training in Ireland, Programme Director for Basic Specialist Training with RCPI, and as a past President of the Irish Society for Rheumatology.
PUBLISHED ARTICLES
“Rheumatic disease differentiation using immunoglobulin G sugar printing by high-density electrophoresis”: Published in The Journal of Rheumatology, this study reflects her in-depth investigation into rheumatic diseases.
“Benefits of exercise in patients with rheumatoid arthritis: a randomized controlled trial”: This research work, highlighting the positive impact of exercise on rheumatoid arthritis, underscores Prof. Cunnane’s dedication to practical, patient-centered research.
Additionally, Prof. Cunnane has made notable contributions to the Annals of the Rheumatic Diseases, discussing early referral, diagnosis, and treatment of rheumatoid arthritis. She has also been involved in a study on the NCBI platform investigating exercise benefits in rheumatoid arthritis patients.
Professor Gaye Cunnane’s career is a testament to her commitment to improving patient outcomes in rheumatology through rigorous research, clinical excellence, and dedicated teaching. Her work continues to influence the field of rheumatology, both in Ireland and internationally.